Big Pharma, Corruption, Medical Research & Your Health
- Joan Rothchild Hardin

- Aug 8, 2015
- 19 min read
Updated: Sep 1, 2021

BIG PHARMA
Peter Rost, MD, worked in medical advertising before moving into the pharmaceutical and biotech industry in 1992. Among the positions he has held are Vice President for Marketing in the Women’s Healthcare Division at Wyeth Pharmaceuticals, Vice President for Marketing and Endocrine Care at the Swedish pharmaceutical and biotechnological company Pharmacia, and Vice President for Marketing at multinational pharmaceutical giant Pfizer.
Rost turned whistleblower on the entire pharmaceutical industry after becoming concerned about unethical, illegal, and even criminal practices he’d observed at Wyeth and Pfizer .

Published in 2006, The Whistleblower: Confessions of a Healthcare Hitman is his insider’s exposé of the pharmaceutical industry. Amazon’s description of the book: A number of books critical of the pharmaceutical industry have recently been published, but none has been an exposé written by a senior executive of one of the world’s largest pharmaceutical companies. The Whistleblower is at once an unmasking of how corporations take care of malcontents and a gripping story of one man’s fight to maintain his family and his sanity. Starting in 2003, the book details the illegal, even criminal business practices the author witnessed at his corporation, as well as his crusade to legalize the reimportation of drugs. It also explains how in this post-Enron world whistle-blowers can’t simply be fired, and what the author’s corporation did to coerce and silence him. A story of a battle that continues today, one which any American who takes or will take prescription drugs has a stake in, The Whistleblower is a powerful testimony.

Below is a short video of Rost speaking about the close ties between the pharmaceutical industry and the medical profession. The clip is from a documentary called ONE MORE GIRL, about Gardasil, a vaccine developed by Merck to prevent the sexually transmitted Human Human Papillomavirus (HPV). The tag for Gardasil ads is variations on “I want to be one less girl who battles cervical cancer.”
Since Gardasil was introduced, thousands of girls have had adverse reactions to it and it has killed over 100 girls. Reactions to the vaccine have included strokes, seizures, dizziness, fatigue, weakness, headaches, stomach pains, muscle pain and weakness, joint pain, auto-immune problems, chest pains, hair loss, appetite loss, personality changes, insomnia, hand and leg tremors, arm and leg weakness, shortness of breath, heart problems, paralysis, itching, rashes, swelling, aching muscles, menstrual cycle changes, fainting, swollen lymph nodes, night sweats, nausea, temporary vision/hearing loss. (The Truth About Gardasil, undated) The US FDA approved use of the vaccine in 2006, recommending vaccination before adolescence. Gardasil is now being recommended for boys as well as girls.

One of Gardasil’s lead researcher developers, HPV expert, and Merck insider, Dr Diane Harper, notes that the vaccine has not been shown to prevent cervical cancer. “95% of women who are infected with HPV never even get cervical cancer. It seemed odd to be mandating something which 95% of infections never amount to anything. Pap smear screening is far and away the biggest thing a woman can do to protect herself to prevent cervical cancer.”
Dr Harper also points out that Merck’s marketing campaign was designed to scare parents into getting their children vaccinated. “If parents and girls were told the benefits and harms of Pap screening and HPV vaccines, an informed and valued decision would have been able to be made.” (Landis, 2013)
The CDC recommends a three-dose series of HPV vaccination for all 11 or 12 year old children. At least 25 states and territories have already enacted legislation making HPV vaccinations mandatory for girls entering 6th or 7th grade. (National Conference of State Legislatures, 2015)
Here are some of Big Pharma’s unsavory practices – draw your own conclusions:
21 TOP BIG PHARMA COMPANIES

PROFITS OVER DRUG EFFECTIVENESS & SAFETY
Here’s but one example of a much broader problem: childhood vaccines. Robert F. Kennedy, Jr., recent article, Children at Risk – Vaccines, Government & Big Pharma’s Dirty Money, reveals that, as of 2013, the Centers for Disease Control and Prevention (CDC) had 271 new vaccines under development. If approved, this would bring $100 billion in vaccine revenues into the coffers of pharmaceutical companies by 2025. As it is, the CDC’s recommended vaccination schedule calls for 49 doses of 14 different vaccines between birth and age 6. Most babies in the US receive over 24 vaccines by their first birthdays and most children here get a minimum of 56 doses of 14 vaccinations by age 18. This in spite of the CDC’s acknowledging that vaccines can have dangerous side effects and are sometimes fatal. (England, 2015) A 2011 study found that developed nations, like the US, which administer the largest number of vaccinations in the first 12 months of life, have the highest infant mortality rates. (Mercola, 2011)

Kennedy wrote of the CDC (England, 2015): “Public health may not be the sole driver of CDC decisions to mandate new vaccines. Four scathing federal studies, including two by Congress, one by the U.S. Senate, and one by the HHS Inspector General, paint CDC as a cesspool of corruption, mismanagement and dysfunction with alarming conflicts of interest suborning its research, regulatory and policymaking functions. CDC rules allow vaccine industry profiteers like Dr. Offit to serve on advisory boards that add new vaccines to the schedule. In a typical example, Offit in 1999 sat on the CDC’s vaccine advisory committee and voted to add the rotavirus vaccine to CDC’s schedule, paving the way for him to make a fortune on his own rotavirus vaccine. Offit and his business partners sold the royalties to his rotavirus vaccine patent to Merck in 2006 for $182 million. Offit told Newsweek, ‘It was like winning the lottery!’” This is the CDC’s recommended vaccination schedule for children from birth to 18 years: BIRTH (12 hours)
Hepatitis B
2 MONTHS
Diphtheria
Tetanus
Pertussis
Polio
HIB
Rotavirus
Hepatitis B
PCV
4 MONTHS
Diphtheria
Tetanus
Pertussis
Polio
HIB
Rotavirus
PCV
6 MONTHS
Diphtheria
Tetanus
Pertussis
Polio
Rotavirus
Hepatitis B
PCV
Influenza
7 MONTHS
Influenza
12 – 18 MONTHS
Diphtheria
Tetanus
Pertussis
Measles
Mumps
Rubella
HIB
PCV
Varicella
Hepatitis A
2 – 6 YEARS
Diphtheria
Tetanus
Pertussis
Polio
Measles
Mumps
Rubella
Varicella
Influenza
7-18 YEARS
Diphtheria
Tetanus
Pertussis
Influenza
HPV
Meningococcal
MULTIPLE VACCINATIONS GIVEN SIMULTANEOUSLY
“In 1983, the CDC directed doctors to give a child no more than 4 vaccines (DPT, polio) simultaneously. By 2013, the CDC directed that a child can receive 8 or more vaccines at once.
“The Institute of Medicine published a report in 2013 stating that ‘key elements of the entire [child vaccine] schedule – the number, frequency, timing, order and age of administration of vaccines – have not been systematically examined in re- search studies.’”
VACCINATIONS DURING PREGNANCY
“A new CDC policy directs doctors to give pregnant women one dose of influenza vaccine in any trimester and one dose of pertussis containing Tdap vaccine after 20 weeks during every pregnancy. The U.S. Food and Drug Administration (FDA) has determined that there are no adequate, well controlled studies conducted in pregnant women to determine if it is safe for the developing fetus or pregnant woman to receive Tdap and Influenza vaccines during pregnancy.”
Source: National Vaccine Information Center, 2013
And the CDC is considering adding even more vaccines to this list – possibly as many as 271?

HOW BIG PHARMA INFLUENCES DOCTORS

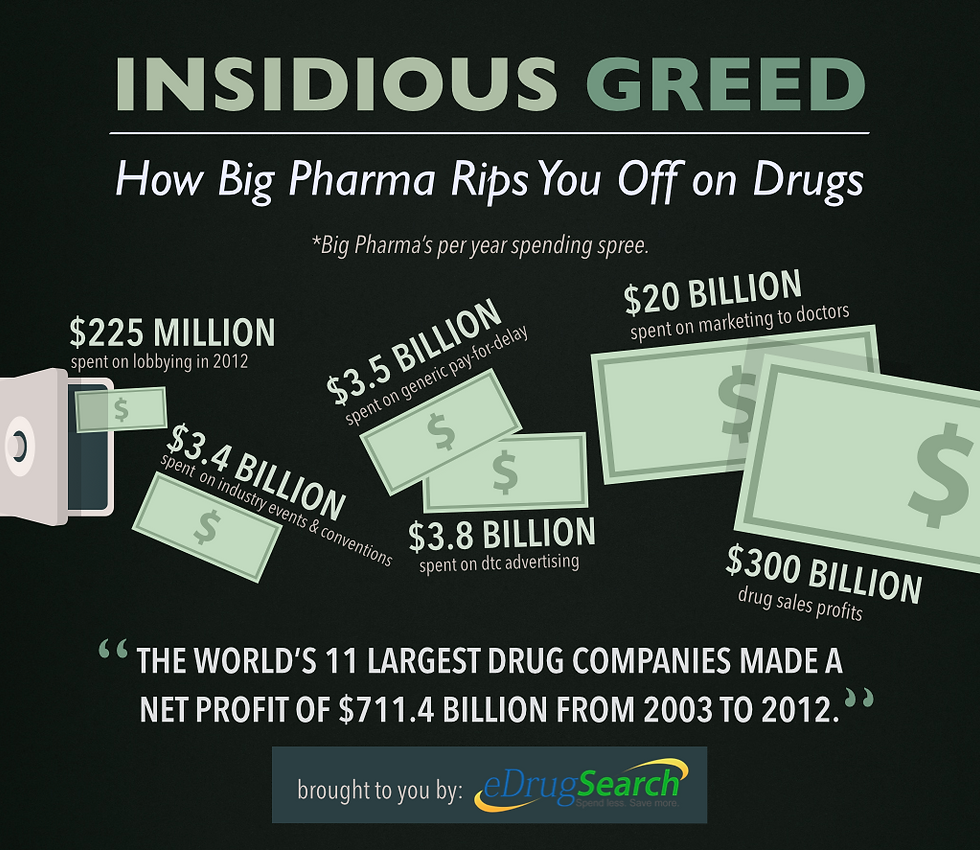
Recently mandated data collected by the US Department of Health and Human Services shed light on the cozy relationship between doctors and the health care industry. Pharmaceutical and medical device companies made 4.4 million payments to 500,000 health care professionals and teaching hospitals — adding up to a total of almost $3.5 billion. The table below breaks down the amounts: Lucrative Relationships Pharmaceutical and medical device companies made payments of $3.48 billion to doctors and other health care professionals in the five-month period from 8/1-12/31/2013. (Thomas et al, 2014) PURPOSE AMOUNT Research payments $1.49 billion Ownership interest 1.02 billion Speaking and consulting fees 380 million Royalties and licenses 302 million Travel, food, lodging 167 million Other 128 million TOTAL $3.48 billion Source: U.S. Department of Health & Human Services “Big Pharma spends almost $20 billion annually marketing their products to doctors, which yields profits upwards of $300 billion per year in drug sales. A handful of these doctors were paid more than $500,000 apiece. Others were paid millions for the drugs and devices they helped to create. Doctors insist that this money doesn’t influence what they recommend to their patients. However, it’s extremely difficult to imagine what purpose the payments would serve if not to increase product sales through prescriptions.” (Byrd, 2014) Dr. Michael Carome, Director of Public Citizen’s Health Research Group, commented: “When you look at why do drug companies and device companies make gifts and offer consulting payments and honoraria to physicians, the main goal is to influence prescribing practices. The interest of those companies is to improve their financial bottom line, and not necessarily represent the best interest of patients.” (Thomas et al, 2014) PHARMA SPENDS MORE ON MARKETING THAN ON RESEARCH & DEVELOPMENT

The World Health Organization (WHO) states: “The global pharmaceuticals market is worth US$300 billion a year, a figure expected to rise to US$400 billion within three years. The 10 largest drugs companies control over one-third of this market, several with sales of more than US$10 billion a year and profit margins of about 30%. Six are based in the United States and four in Europe. It is predicted that North and South America, Europe and Japan will continue to account for a full 85% of the global pharmaceuticals market well into the 21st century. Companies currently spend one-third of all sales revenue on marketing their products – roughly twice what they spend on research and development. “As a result of this pressure to maintain sales, there is now … an inherent conflict of interest between the legitimate business goals of manufacturers and the social, medical and economic needs of providers and the public to select and use drugs in the most rational way. This is particularly true where drugs companies are the main source of information as to which products are most effective.” (WHO, 2015) John Oliver

BIG PHARMA PAYS SCIENTISTS FOR GHOSTWRITTEN PAPERS

It’s well known that drug companies have a practice of paying large sums of money to physicians at elite medical centers and other experts in their fields to allow themselves to be listed as the “authors” of articles endorsing new drugs – articles actually written by ghostwriters (people employed by the companies manufacturing the drugs) and which the “authors” had no hand in either researching or writing. For a ghostwritten article, the actual author is not named in the final published manuscript, only the well-known recruited physician or expert who has had limited or zero involvement with any aspect of the research – from clinical trial, study design, methods, data collection and analysis, or writing of the manuscript. The named author may have been allowed to look at tables compiled by the company employee but has probably not ever seen the study’s raw data. “Ghostwriting is part of a larger scheme called ‘publication planning,’ a process by which pharmaceutical, biotechnology, medical device, and medical supply companies produce, publish, and release articles in medical journals, abstracts and posters at conferences, meetings, and symposia, to establish key marketing messages. This process is closely monitored to ensure that the sponsoring companies’ medications are being effectively promoted. This process has been known to disseminate information embedded with factual errors, misrepresentation, overstated benefits, and understated risks of medications being promoted.” (Shnier, 2014) Dr David Healy, a British psychopharmacologist, said in 2002, “It may well be that 50% of the articles on drugs in the major journals across all areas of medicine are not written in a way that the average person in the street expects them to be authored.” (Boseley, 2002) The practice has only increased since then. Ghostwriting has become especially widespread in medical fields where drugs play a major role in treatment, such as cardiology and psychiatry. Senator Charles Grassley (R-Iowa), who has been leading a long-running investigation into conflicts of interest in medicine, put pressure on the National Institutes of Health to stop the practice of ghostwriting. In response to Grasley’s exposure of cases where leading medical researchers neglected to report monies received from pharmaceutical and medical device companies, in 2010 the NIH proposed improved disclosure guidelines for federal grant recipients. (Grassley, 2010) A “Sunshine Act” was enacted into law by Congress in 2010 and implemented in 2013 as part of the Patient Protection and Affordable Care Act, familiarly referred to as Obamacare. Under the PPACA, pharmaceutical, medical device, and medical supply manufacturers must report payments and exchanges of value each year. Those companies have questioned exactly which “exchanges of value” require disclosure. (Shnier, 2014) One of the contested areas is whether companies are required to disclose “medical writing support provided by pharmaceutical companies to authors of clinical studies” and “editorial services.” BIG PHARMA’S INFLUENCE ON MAJOR MEDICAL JOURNALS
Dr Ben Goldacre, an epidemiologist and author of Bad Science: Quacks, Hacks, and Big Pharma Flacks (2010) and Big Pharma: How Drug Companies Mislead Doctors and Harm Patients (2014), discovered that drug companies funnel $10 – 20 million annually to major medical journals such as the New England Journal of Medicine and the Journal of the American Medical Association. He notes it’s therefore not surprising that studies funded by the pharmaceutical industry are more likely to make it into print in these influential journals. (Goldacre, 2014). FDA IN BED TOGETHER WITH BIG PHARMA

Medical and Organizational Sociologist Donald W. Light’s 2013 paper, entitled “Institutional Corruption of Pharmaceuticals and the Myth of Safe and Effective Drugs”, presented damning evidence against the US Food and Drug Administration for failing to scrutinize the safety and efficacy of new drugs adequately before allowing them to be marketed.
After compiling his data and noting that almost all the new drugs the agency approved over the previous 30 years were little or no better than drugs already on the market, Light concluded the FDA “cannot be trusted”, that the agency has become a pay-for-play front group catering to the interests of the pharmaceutical industry. FDA approval of old drugs repackaged with only minor changes allows companies to renew their patents and reap new record-profits. Patents typically last 20 years from the date of filing.
Drug companies provide the major source of the FDA’s funding so the agency has succumbed to pressure to speed up the approval process for bringing new drugs to market – putting patients at increased risk.
Light’s report points out that prescription drugs, used as directed, kill at least 125,000 people annually yearly, making them the fourth leading cause of death in the US. Tens of thousands more are hospitalized each year from adverse effects from prescription drugs.
“[O]ver the past 30 years, approved drugs have caused an epidemic of harmful side effects, even when properly prescribed,” explains a preface to the Harvard report. “Every week, about 53,000 excess hospitalizations and about 2,400 excess deaths occur in the United States among people taking properly prescribed drugs to be healthier.”
“The FDA in effect serves as the re-generator of patent-protected high prices for minor drugs in each disease group, as their therapeutic equivalents lose patent protection,” explains the report. “The FDA routinely approves scores of new minor variations each year, with minimal evidence about risks of harm. … One in every five drugs approved ends up causing serious harm.”
Light’s paper was published in a special issue of the Journal of Law, Medicine & Ethics. (Huff, 2013)

MEDICAL FIELD IN BED WITH PHARMA – MORE EVIDENCE Dr Marcie Angell is currently Senior Lecturer in Social Medicine at Harvard Medical School and was the Editor-in-Chief of the New England Journal of Medicine for two decades. Her January 15 2009 New York Review of Books article, “Drug Companies & Doctors: A Story of Corruption”, is worth looking at. It discusses three books on the corrupt doings of Big Pharma, their adverse effects on the practice of medicine and our health: Side Effects: A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial by Alison Bass. This is the story of how British drug giant GlaxoSmithKline buried evidence that Paxil, its best-selling antidepressant, was ineffective and possibly harmful to children and teens. Our Daily Meds: How the Pharmaceutical Companies Transformed Themselves into Slick Marketing Machines and Hooked the Nation on Prescription Drugs, by Melody Petersen. This book and and the one below are about drug companies’ highly effective tactic of creating newly identified conditions with serious-sounding quasi-medical names that seem to require long-term treatment with their drugs. As examples: we’re being bombarded by ads for drugs to help us with Gastro-esophageal reflux disease, Social Anxiety Disorder, Premenstrual Dysphoric Disorder, Erectile dysfunction. “Ask your doctor.” Shyness: How Normal Behavior Became a Sickness by Christopher Lane

These three books cover such unsettling topics as the financial ties between Big Pharma and the academic physicians who play a large role in setting the market value of prescriptions drugs, sloppy research, unapproved and dangerous off-label use of pharmaceutical, huge speaking and consulting fees pharmaceutical companies pay to some physicians who routinely prescribe their drugs, the serious conflict of interest practice of allowing drug companies to pay researchers to test their products. There’s more – all of it involving huge sums of money and quite unsavory
Dr Angell concludes her review:
“After much unfavorable publicity, medical schools and professional organizations are beginning to talk about controlling conflicts of interest, but so far the response has been tepid. They consistently refer to “potential” conflicts of interest, as though that were different from the real thing, and about disclosing and “managing” them, not about prohibiting them. In short, there seems to be a desire to eliminate the smell of corruption, while keeping the money. Breaking the dependence of the medical profession on the pharmaceutical industry will take more than appointing committees and other gestures. It will take a sharp break from an extremely lucrative pattern of behavior. But if the medical profession does not put an end to this corruption voluntarily, it will lose the confidence of the public, and the government (not just Senator Grassley) will step in and impose regulation. No one in medicine wants that.”
(Angell, 2009)

“MOST PUBLISHED RESEARCH FINDINGS ARE FALSE”
As if the revelations about Big Pharma aren’t bad enough, it also appears that much of the medical research that gets published and forms the basis of medical practice is seriously flawed.

John Ioannidis MD is currently Professor of Health Research and Policy at Stanford School of Medicine, the University’s Rehnborg Chair in Disease Prevention and Director of its Prevention Research Center, as well as Co-Director of the Meta-Research Innovation Center at Stanford.
Ioannidis and other experts point out there is considerable evidence showing severe flaws in the science underlying medical education and pharmaceutical development.
Ioannidis is one of the world’s most respected experts on the credibility of medical research. He and his team have found problems in the science behind as much as 90% of the published medical information doctors rely on when prescribing medications, recommending tests and surgical procedures, and advising patients on dietary practices. (Freedman, 2010)

In the early 1990’s Ioannidis, was starting out as a physician and researcher at Harvard. He was also a math whiz and decided to apply rigorous statistical analytic procedures to the research data he presumed backed up doctors’ treatment decisions. “I assumed that everything we physicians did was basically right, but now I was going to help verify it,” he says. “All we’d have to do was systematically review the evidence, trust what it told us, and then everything would be perfect.” What he discovered shocked him: There was a great deal of published research but much of it was quite sloppily done. Many of the studies were based on observations of only a small number of cases. He also noted that many research findings in all areas of medical research were refuted by later studies. Hardly compelling scientific evidence to underpin the practice of medicine.

“I realized even our gold-standard research had a lot of problems,” he says. So he began looking for the specific ways in which studies were going wrong and discovered an astonishing range of errors: Problems in the ways researchers posed their research questions, skewed selection of study participants, use of seriously flawed research designs and measurements of their test variables, faulty analyses of their data, poor presentation of the results, problems with how studies were chosen for or denied publication in medical journals. Ioannidis realized a serious dysfunction underlay these flaws. “The studies were biased,” he says. “Sometimes they were overtly biased. Sometimes it was difficult to see the bias, but it was there.” We tend to think scientific research is an objective and rigorous process but that’s often not the case. Researchers undertake studies hoping to find particular results – they want their hypotheses to be shown to be true. And it’s easy to manipulate results, intentionally or unconsciously. “At every step in the process, there is room to distort results, a way to make a stronger claim or to select what is going to be concluded,” says Ioannidis. “There is an intellectual conflict of interest that pressures researchers to find whatever it is that is most likely to get them funded.” (Freedman, 2010) By the late 1990’s, he and his team began publishing a series of papers pointing out the specific ways medical researchers were obtaining misleading results. By this time, he was no longer the only meta-researcher calling attention to the high rate of errors in medical literature. But he was determined to present his findings in a way that would demonstrate the seriousness of the problem.

In 2005 Ioannidis published his findings as “Why Most Published Research Findings Are False”. This article became the most widely accessed article in the history of the online medical journal PLoS (the Public Library of Science). In the PLoS paper, Ioannidis presented a detailed mathematical proof that researchers will arrive at incorrect findings most of the time. Factors going into this calculation were: Researcher bias, flawed research techniques, the tendency to study career-advancing topics rather than use good science to test more plausible hypotheses, and using the peer-review process to bar opposing views from getting published. (Freedman, 2010) (Ioannidis, 2005-B) From Ioannidis’s summary of his PLoS paper: “There is increasing concern that most current published research findings are false. … Simulations show that for most study designs and settings, it is more likely for a research claim to be false than true. Moreover, for many current scientific fields, claimed research findings may often be simply accurate measures of the prevailing bias.” Take a look at the PLoS article if you want to see how he reached the conclusion that “most published research findings are false”. Professor Doug Altman, a UK researcher and Director of the Oxford Centre for Statistics in Medicine, says of Ioannidis’ conclusions, “You can question some of the details of John’s calculations, but it’s hard to argue that the essential ideas aren’t absolutely correct.” (Freedman, 2010)

Ioannidis published a second paper, called “Contradicted and Initially Stronger Effects in Highly Cited Clinical Research”, that same year in the Journal of the American Medical Association. This one is a meta-analysis of original clinical research studies on medical intervention effectiveness published in the three major general clinical journals (New England Journal of Medicine, JAMA, Lancet) and in the 17 highest-impact specialty journals between 1990-2003. Articles had to have been cited over 1,000 times in the medical literature to be included in the analysis. (Ioannidis, 2005 -A) For this paper, Ioannidis and his team compared the results of these highly-cited articles against studies of about the same or larger sample size and similar or better-controlled designs. They also performed the same comparative analysis for matched studies that had been less frequently cited to see if the findings and potential for contradiction of highly-cited studies differed from less frequently studies. Their meta-analysis included these findings:
45 of 49 highly-cited original studies claimed their interventions were effective. Of these 45, the results of 16% of them were contradicted by later studies. Subsequent studies found weaker effects than had been reported in 16% of the original studies. 44% of the studies were later replicated. 24% of them were unchallenged.
84% of the published results in the highly-cited, non-randomized, original studies were later either contradicted or weaker effects were subsequently found.
Matched control studies had about the same share of refuted results as highly-cited studies but included more studies with ‘negative’ results. (* See NOTE on ‘negative findings below.)

Ioannidis points out that “most research publications have little impact while a small minority receives most attention and dominates scientific thinking and clinical practice…. Clinical research on important questions about the efficacy of medical interventions is sometimes followed by subsequent studies that either reach opposite conclusions or suggest that the original claims were too strong. Such disagreements may upset clinical practice and acquire publicity in both scientific circles and in the lay press.” (Ioannidis, 2005-A) Ioannidis’ two 2005 papers challenge the very foundation of conventional medical research and practice. His writings have been published in leading medical journals and are heavily cited.

PERSONAL EXPERIENCE Years ago, when I was reviewing published research on psychosocial aspects of breast cancer for the Stanford Research Institute, my own observations coincided with those Ioannidis discovered. Sometimes the stated research hypothesis being tested was so vague, any results would be meaningless. It was often impossible to tell the basis on which subjects had been selected to be in the research and control groups. Sometimes there wasn’t even a control group. Results were sometimes presented without any description of how they’d been analyzed. The probability level chosen for analyzing the data was often not stated so there was no way to tell if the findings were in any way statistically meaningful.

THE VIEWS OF TWO PROMINENT MEDICAL JOURNAL EDITORS The observations below, from a former and a current Editor-in Chief of two of the world’s best regarded medical journals, lend strong support to Rost and Ioannidis’ claims: “It is simply no longer possible to believe much of the clinical research that is published, or to rely on the judgment of trusted physicians or authoritative medical guidelines. I take no pleasure in this conclusion, which I reached slowly and reluctantly over my two decades as an editor of the New England Journal of Medicine.” – Dr Marcia Angell, physician and longtime Editor-in-Chief of the New England Medical Journal (Marcovitch, 2010) “The case against science is straightforward: much of the scientific literature, perhaps half, may simply be untrue. Afflicted by studies with small sample sizes, tiny effects, invalid exploratory analyses, and flagrant conflicts of interest, together with an obsession for pursuing fashionable trends of dubious importance, science has taken a turn towards darkness.” – Dr Richard Horton, the current Editor-in-Chief of the Lancet (Walia, 2015) A NOTE ON ‘NEGATIVE’ FINDINGS The Null Hypothesis

The Null Hypothesis states there is no significant relation or difference between two variables so no good reason for changing our thinking about how they relate to each other. In scientific study, researchers are trying to REJECT the Null Hypothesis by demonstrating grounds for believing their Alternative Hypothesis has merit – that a significant relationship DOES EXIST between the phenomena or groups they’ve studied – (eg, that treatment with a potential drug has a measurable effect). If the research results don’t reject the Null Hypothesis, then nothing new or surprising has been discovered. Studies that fail to find positive results are harder to publish. For instance, you set out to show that a particular drug lowers blood pressure and don’t find evidence that it does. Not very sexy – or publishable in a major journal. The authors of an article entitled “Negativity towards negative results: a discussion of the disconnect between scientific worth and scientific culture” asked the question “What happens when you obtain results that support the null hypothesis, or do not fit with current scientific thinking?” The authors went on to discuss publication bias and the difficulty researchers encounter in communicating negative results. “Negative findings are a valuable component of the scientific literature because they force us to critically evaluate and validate our current thinking, and fundamentally move us towards unabridged science.” (Matosin et al, 2014)

CONCLUSION While all the above is deeply disturbing, it’s also important to remember that some excellent research has been and is currently being done, that pharmaceutical companies also manufacture drugs that have saved many lives and improved the quality of life for many more around the world, and that most physicians are good people with their patients’ best interests at heart.

REFERENCES Angell, M. (1/15/2009). Drug Companies & Doctors: A Story of Corruption. New York Review of Books. See: http://www.nybooks.com/articles/archives/2009/jan/15/drug-companies-doctorsa-story-of-corruption/ Boseley, S. (2002). Scientists Take Money for Ghostwritten Papers: Scandal of scientists who take money for papers ghostwritten by drug companies. The Guardian. See: http://www.theguardian.com/uk/2002/feb/07/research.health1 Byrd, C. (2014). Insidious Greed: How Big Pharma Rips You Off on Drugs. See: https://www.edrugsearch.com/edsblog/how-big-pharma-rips-you-off-on-drugs/#.VcFjPjBVhHw England, C. (2015). Profit over Safety – Centers for Disease Control Names 271 New Vaccinations. See: http://vactruth.com/2015/08/03/271-vaccines-in-development/ Freedman, D. (2010). Lies, Damned Lies and Medical Science: MUCH OF WHAT MEDICAL RESEARCHERS CONCLUDE IN THEIR STUDIES IS MISLEADING, EXAGGERATED OR FLAT-OUT WRONG! The Atlantic. See: http://www.theatlantic.com/magazine/archive/2010/11/lies-damned-lies-and-medical-science/308269/ Goldacre, B. (2014). Big Pharma: How Drug Companies Mislead Doctors and Harm Patients. See: http://www.amazon.com/Bad-Pharma-Companies-Mislead-Patients/dp/0865478066/ref=la_B002C1VRBQ_1_1?s=books&ie=UTF8&qid=1438969537&sr=1-1 Grassley, C. (2010). Grassley releases medical ghostwriting report, recommends NIH promote transparency. See: http://www.grassley.senate.gov/news/news-releases/grassley-releases-medical-ghostwriting-report-recommends-nih-promote-transparency Ioannidis, P.A. (2005-A). Contradicted and Initially Stronger Effects in Highly Cited Clinical Research. JAMA, 294:2, 218-228. See: http://jama.jamanetwork.com/article.aspx?articleid=201218 Huff, E.A. (2013). New Harvard paper slams FDA, says agency ‘cannot be trusted’. See: http://www.naturalnews.com/043265_FDA_Big_Pharma_Harvard_University.html# Ioannidis, P.A. (2005-B). Why Most Published Research Findings Are False. PLos – Medicine. See: http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124 Landis, M. (2013). Be One Less, Say No to Gardisil! See: http://doyourhw.org/2013/02/06/be-one-less-say-no-to-gardisil/ Marcovitch, H. (2010). Editors, Publishers, Impact Factors, and Reprint Income. PLoS – Medicine. See: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2964337/ Matosin, N. et al. (2014). Negativity towards negative results: a discussion of the disconnect between scientific worth and scientific culture. Disease Models & Mechanisms, 7:2, 171–173. See: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3917235/ Mercola, R. (2011). What Every Parent Must Know: This Occurs Before the Age of 6. http://articles.mercola.com/sites/articles/archive/2011/11/03/right-vaccine-dosage-for-babies.aspx National Conference of State Legislatures. (2015). HPV VACCINE POLICIES. See: http://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx National Vaccine Information Center. (2013). 49 DOSES OF 14 VACCINES BEFORE AGE 6? 69 DOSES OF 16 VACCINES BY AGE 18? Before you take the risk, find out what it is. See: http://www.nvic.org/CMSTemplates/NVIC/pdf/49-Doses-PosterB.pdf Rost, P. (2006). The Whistleblower: Confessions of a Healthcare Hitman. See: http://www.amazon.com/Whistleblower-Confessions-Healthcare-Hitman/dp/193336839X/ref=sr_1_1?s=books&ie=UTF8&qid=1438448480&sr=1-1&keywords=whistleblower+peter+rost Shnier, A. (2014). How much do companies pay for ghostwritten articles?: Drug companies against disclosure of payments for ghostwriting under US Sunshine Act. See: http://adrienneshnier.com/1/post/2014/02/how-much-do-companies-pay-for-ghostwritten-articles-drug-companies-against-disclosure-of-payments-for-ghostwriting-under-us-sunshine-act.html The Truth About Gardasil. (undated). See: http://truthaboutgardasil.org/ Thomas, K. et al. (9/30/2014). Detailing Financial Links of Doctors and Drug Makers. New York Times. See: http://www.nytimes.com/2014/10/01/business/Database-of-payments-to-doctors-by-drug-and-medical-device-makers.html Walia, A. (2015). Editor In Chief Of World’s Best Known Medical Journal: Half Of All The Literature Is False. See: http://www.collective-evolution.com/2015/05/16/editor-in-chief-of-worlds-best-known-medical-journal-half-of-all-the-literature-is-false/ World Health Organization (WHO). (2015). Pharmaceutical Industry. See: http://www.who.int/trade/glossary/story073/en/ © Copyright 2015 Joan Rothchild Hardin. All Rights Reserved.
DISCLAIMER: Nothing on this site or blog is intended to provide medical advice, diagnosis or treatment.


Comments